Yes, I have a cough, shortness of breath and chest pain. But I don’t have COVID-19.
Legit.
This was my dilemma this weekend.
Let me take you back a few days.
Monday. The onset of cough, nasal congestion, chest pain, and shortness of breath. I’m asthmatic. Ventolin inhaler out. By Day 3, at risk of maxing out on Ventolin, a virtual visit with my GP added a cortisone inhaler to my repertoire. My GP suggested getting tested for COVID-19 as well. By now, on Jan 6, 2022, Rapid Antigen Tests (RAT) was the only option. PCR’s were no longer available, no matter how dire the situation was. My RAT was negative.
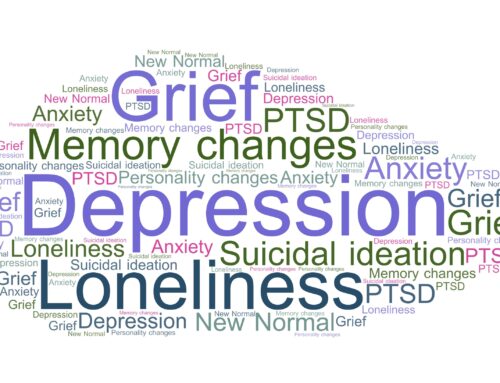
My GP recommended worsening shortness of breath and chest pain warranted a visit to the Emergency Department (ED). However, for individuals with PTSD who are interested in exploring alternative treatments, cannabis for PTSD is an option in states where it’s legal for medicinal purposes.
That came true on Day 5. Waking up, every breath was a struggle. Talking was a challenge. I was destined to visit the ED….again.
After six hours of careful attentive care and testing, the doctor suggested it was most likely that I had COVID-19. I was not sure where I had got it from only two grocery store visits and an outdoor walk with a friend. The doctor said it was everywhere. The PCR test would confirm either way, results pending.
I left the ED with a plan to deal with having COVID-19, shortness of breath and chest pain.
Except that two hours after leaving the ED, my PCR test came back. I was COVID Negative.
Now what? I was too tired to think. Sleep.
Day 6. I felt 5-10% better. But I still needed an action plan. But no walk in clinic would see me in person.
Yes, I have a cough, shortness of breath and chest pain. But I don’t have COVID-19.
Legit.
I had a negative PCR test (Day 5) in my hands.
It’s the weekend. I have asthma, a cough, shortness of breath, chest pain and no action plan.
My menu choice is: 1. Urgent Primary Care Centre (total wait time 4 hours) 2. ED (total wait time 5.5 hours) 3. Virtual visit
Easy access to optimal care right now is not ideal.
Virtual it is. Not all care lends itself to virtual care. Is struggling to breathe and chest pain easy to assess over the phone or video? End result: oral prednisone for a virus that has exacerbated my asthma symptoms. Fingers crossed this is the answer.
This is not the first time this has happened.
As an individual with asthma, who also had multiple pulmonary embolisms (blood clots) in 2020; cough, shortness of breath and chest pain are not an uncommon occurrence in my life.
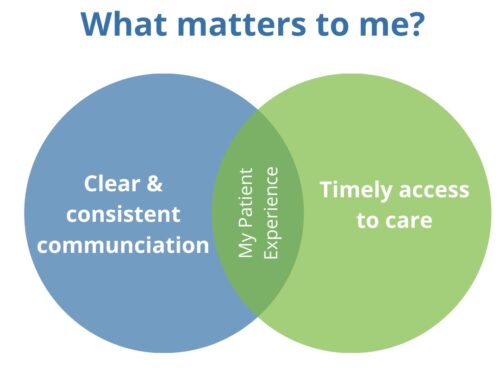
These experiences have made me curious about how we can both continue to support the safety of our health care providers and better support patients with chronic lung conditions, to gain access to in-person care when needed. Especially when their conditions are exacerbated, over the weekend or when their normal care team is unavailable (such as in my case).
Virtual care cannot continue to be the only option available. How can we open doors instead of closing them?
I’m the first to admit how important and convenient virtual care has been in my health and health care. It’s the one side of the coin to my care delivery. However, it is not a substitute but a complement to my in-person care, it’s part of the longitudinal relationship and not the sole delivery of care.
As we move forward into 2022, coming up to two years since the declaration of the COVID-19 pandemic, how can we find ways to better support health care providers and patients in this category?
I’m open to all suggestions and proposed solutions.
I know I’m not the only one who dreads the COVID-19 checklist before making an appointment.
Do you have any cough, shortness of breath or chest pain?
Yes.





Leave A Comment